Public Health Hindsight: How Well Did Korea Handle its MERS Outbreak?
South Korea vaulted into international news this summer when its outbreak of Middle East Respiratory Syndrome coronavirus, better known as MERS, began making headlines after the first case was identified on May 20. Images of Koreans wearing face masks peppered social media feeds and every major news website.
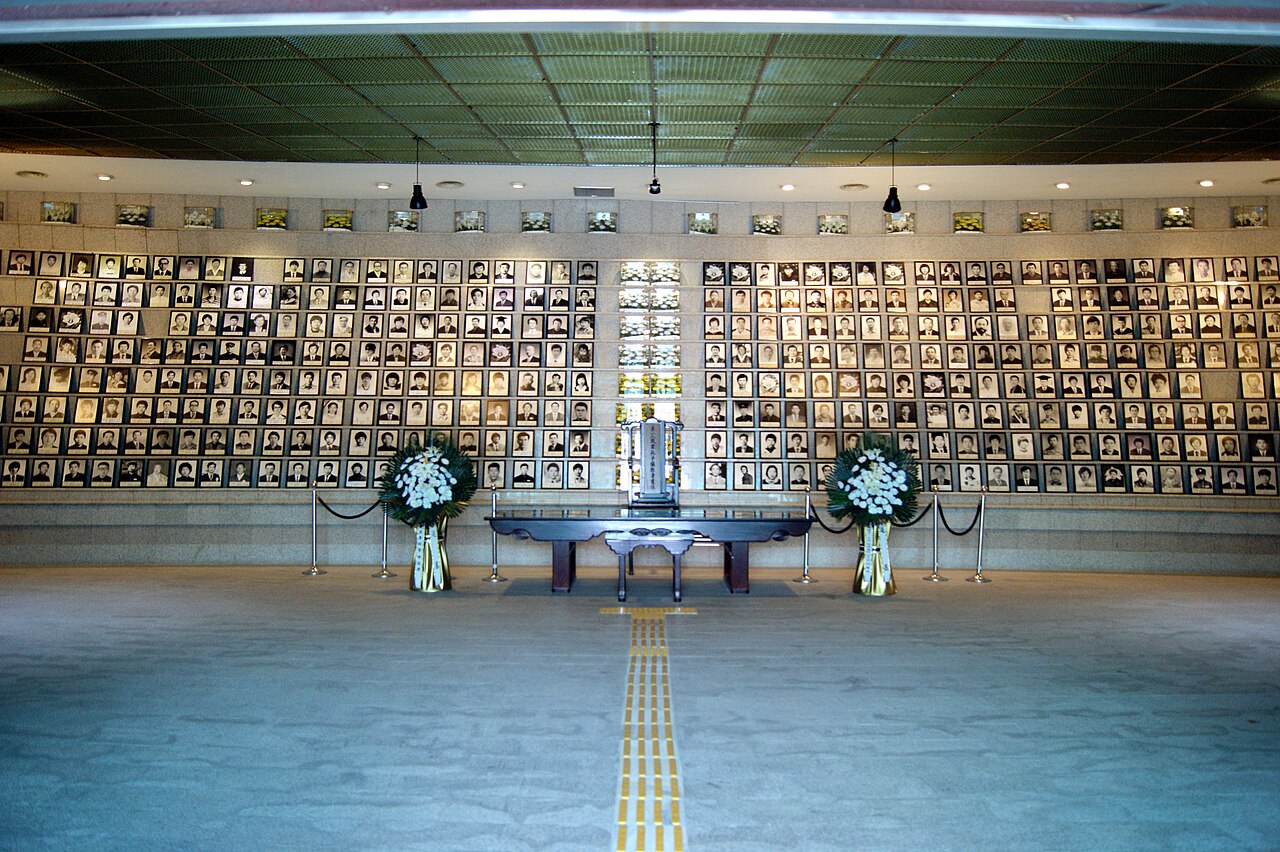
The story dominated headlines throughout June as cases spiked and deaths continued to climb, then ended abruptly in early July as the epidemic was snuffed out, nearly as quickly as it began. There were 185 confirmed cases and 36 deaths by the time the outbreak was declared over on July 28.
World Health Organization Director, Dr. Margaret Chan, was mostly supportive of the government’s response. “After a slow start, the government put in place one of the strongest responses I’ve seen,” she told the Associated Press.
Other commentators were much less generous. A joint panel of experts identified both a failure to provide transparent and rapid distribution of information and a failure to establish proper governance by the administration.
Factors that contributed to the outbreak included doctors’ unfamiliarity with MERS, overcrowded emergency rooms, the practice of “doctor shopping” and the fact that hospital rooms are often bustling with visitors. Nearly 70 percent of the reported cases were among patients, staff and visitors to two hospitals – Samsung Medical Center and Pyeongtaek St. Mary’s Hospital – and the government’s withholding of this information, which it claims it did to prevent panic, only made things worse.
Foreign Policy’s scathing (and cleverly-titled) article, “NightMERS,” identified two major issues to explain why things went so badly. First, the financial strain on the country’s public health care system has led to cost-cutting measures like overreliance on private hospitals (which are much less willing to take aggressive measures to protect public health), insurance only covering shared rooms and low coverage rates for bedside care (leading to family members attending patients, rather than clinicians).
However, the piece did not spare South Korean President Park Geun-hye’s administration, describing a poorly-organized response to the outbreak that allowed the infection to spread without epidemiologic controls. The article stated the following: “Instead of establishing a centralized control tower … five different task forces emerged in different parts of the government, with little coordination … As public distrust of the government grew in reaction to this bungled response, local leaders such as Seoul’s mayor clamored to take over the MERS response in their jurisdictions, which added to the chaos.”
There are always lessons to be learned from mistakes, such as a poorly-handled outbreak, because failures expose weaknesses in systems that can be strengthened, improved or even redesigned. In South Korea’s case, however, it may take more than examining what went wrong. The MERS outbreak is just another example, like the Sewol Ferry Disaster, of the current administration’s poor leadership in times of crisis. Swift and scientifically-informed actions are crucial in disaster response situations – and no doubt a better solution than quarantining the zoo’s camels.